INEB RECENT PUBLICATION: Inflammation in intervertebral disc degeneration and regeneration
INEB researchers recently published an article in the Journal of the Royal Society Interface, available since 11 February 2015. The article is entitled "Inflammation in intervertebral disc degeneration and regeneration" and is authored by Molinos M, Almeida CR, Gonçalves RM, Caldeira J, Cunha C, Barbosa MA.
Intervertebral disc (IVD) degeneration is one of the major causes of low back pain, a problem with a heavy economic burden, which has been increasing in prevalence as population ages. Deeper knowledge of the complex spatial and temporal orchestration of cellular interactions and extracellular matrix remodeling is critical to improve current IVD therapies, which have so far proved unsatisfactory. Inflammation has been correlated with degenerative disc disease but its role in discogenic pain and hernia regression remains controversial. The inflammatory response may be involved in the onset of disease, but it is also crucial in maintaining tissue homeostasis. Furthermore, if properly balanced it may contribute to tissue repair/regeneration as has already been demonstrated in other tissues. In this review, we focus on how inflammation has been associated with IVD degeneration by describing observational and in vitro studies as well as in vivo animal models. Finally, we provide an overview of IVD regenerative therapies that target key inflammatory players.
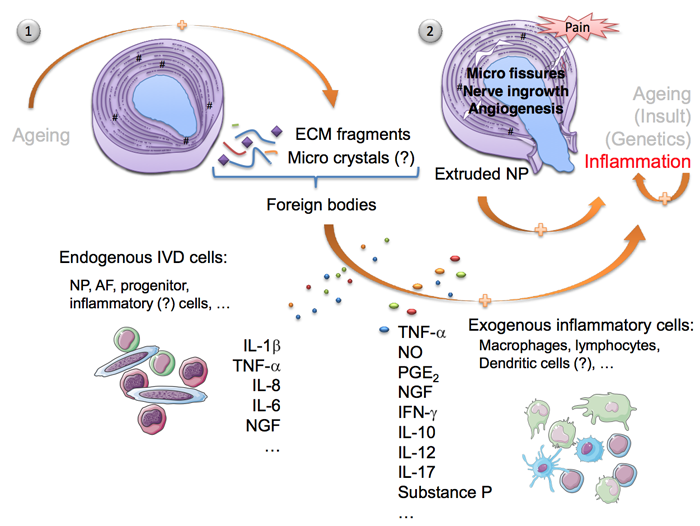
Legend: Inflammation in the IVD. It is unclear whether inflammation is the cause or consequence of disc degeneration and herniation, and what may trigger activation and recruitment of different immune cells. The normal ageing process allied to some genetic pre-disposition causes the IVD to degenerate giving rise to profound changes in the ECM—loss of proteoglycan content, dehydration, malnutrition, decrease of native cell population, matrix breakdown and calcifications. In this scenario, the natural response to mechanical loading is compromised and the IVD becomes prone to microfissures and consequent ingrowth of blood and nerve vessels. (1) Disc herniation may also occur when the AF is no longer able to sustain the NP. ECM fragments and microcrystals may internally elicit an inflammatory response, stimulating endogenous IVD cells to produce pro-inflammatory mediators, that will further feed the cascade of tissue degeneration—IL-1β, IL-8, IL-6. (2) NP is recognized as non-self by the immune system. Hence, its exposure (both in microfissures and herniation) may propagate an immunologic response, with recruitment of macrophages, lymphocytes and other possible inflammatory cells, in order to eliminate the foreign body. Discogenic pain has been many times attributed to TNF-α, PGE2, NO and IFN-γ secretion by macrophages, concomitantly with NGF and substance P production, accompanying the processes of nerve ingrowth and angiogenesis inwards the degenerated IVD. Activated B and T lymphocytes are also recruited to the site, contributing to the positive pro-inflammatory feedback loop established. It is not well understood how endogenous IVD cells interact with exogenous inflammatory cells and whether they positively contribute to tissue resorption and regeneration or not. Spontaneous disc regression is currently believed to be a consequence of macrophage activity.